Are Fungal Rashes Contagious? Clearing Up The Mystery For Healthy Skin

When it comes to our skin, keeping it healthy and glowing is a top priority. But what happens when we encounter fungal rashes? Are they something we need to worry about passing on to others?
Fungal rashes, with their annoying itchiness and discomfort, can make us want to dig deep into understanding their contagiousness. In this article, we’re going to dive into what fungal rashes are and find out whether they’re contagious or not. We’ll also explore how to keep our skin clear and healthy.
So, let’s get started!
Table Of Contents
- Understanding Fungal Rashes: Exploring Causes And Types
- Are Yeast Rashes Contagious? Unveiling The Truth
- Home Remedies For Fungal Rashes
- Preventing Fungal Rashes: Tips For Clear and Healthy Skin
- Maintaining Skin Health: Hygiene And Beyond
- How To Deal With A Fungal Rash
- When To Seek Help: Consulting A Professional
- Conclusion: Empowering Healthy Skin Knowledge
Understanding Fungal Rashes: Exploring Causes And Types
Fungal rashes are skin infections caused by different types of fungi. These fungi love warm and moist environments, which is why they often appear in areas of our body like the feet, groin, and armpits.
Fungi are microscopic organisms that can live on the skin, in the air, in soil, and in plants. While many types of fungi are harmless, some can cause infections when they come into contact with our skin. Fungal rashes can vary in appearance and symptoms, but they often lead to redness, itching, and discomfort.
There are two main categories of fungal rashes: yeast infections and fungal skin infections. Yeast infections, often caused by a fungus called Candida, can occur in areas like the mouth (oral thrush) or the genital area (vaginal yeast infections). These rashes are typically not contagious from person to person. On the other hand, fungal skin infections, caused by dermatophytes, can lead to conditions like ringworm, athlete’s foot, and jock itch. These infections can be contagious and spread through direct contact or contact with contaminated surfaces.
List of common fungal infections along with their typical causes
| Fungal Infection | Causes |
| Athlete’s Foot | Fungus (usually Trichophyton) thrives in warm, moist environments like shoes and socks. Common in communal areas like locker rooms. |
| Jock Itch | Similar to athlete’s foot, it occurs in the groin area due to warmth and moisture. |
| Ringworm (Tinea Corporis) | Various types of fungi (e.g., Trichophyton) are transmitted by direct contact with infected humans, animals, or contaminated objects. |
| Nail Fungus (Onychomycosis) | Fungal infection of the nails is often caused by dermatophytes. It can occur due to damp environments and injury to nails. |
| Candidiasis (Yeast Infection) | Candida yeast overgrowth, commonly due to factors like weakened immune system, antibiotics, hormonal changes, and high sugar intake. |
| Oral Thrush | Candida overgrowth in the mouth, often seen in infants, the elderly, and those with compromised immune systems. |
| Vaginal Yeast Infection | Candida overgrowth in the vaginal area, often influenced by hormonal changes, antibiotics, and other factors. |
| Diaper Rash (Candidal Dermatitis) | Candida overgrowth in warm, moist diaper areas, exacerbated by prolonged contact with wet diapers. |
| Tinea Versicolor | Malassezia yeast causing uneven skin pigmentation. More common in humid conditions and in individuals with oily skin. |
| Pityriasis (Tinea) Rosea | Exact cause is unknown, but it might be related to certain viruses or fungi. |
| Sporotrichosis | Caused by the fungus Sporothrix, found in soil and vegetation. Often transmitted through cuts or punctures from plants. |
| Cryptococcosis | Inhalation of Cryptococcus neoformans found in soil contaminated with bird droppings. Mainly affects immunocompromised individuals. |
| Aspergillosis | Inhalation of Aspergillus spores from the environment, common in those with weakened immune systems. |
| Histoplasmosis | Inhalation of Histoplasma capsulatum spores from bird or bat droppings in soil. Endemic in certain regions. |
| Blastomycosis | Inhalation of Blastomyces dermatitidis spores from soil or decaying wood, often affecting outdoor workers. |
| Coccidioidomycosis | Inhalation of Coccidioides immitis or Coccidioides posadasii spores from soil in arid regions. Also known as Valley Fever. |
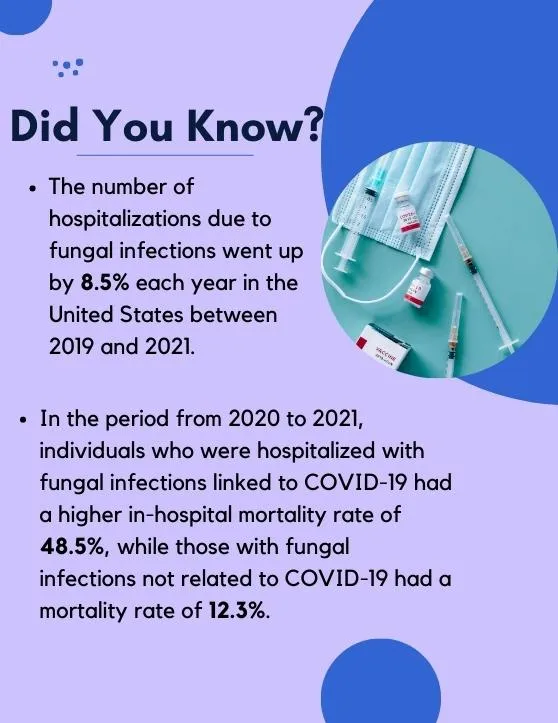
A fungal infection can affect anyone, including individuals with no underlying health issues. Fungi are widespread in our surroundings, and people are exposed to fungal spores through inhalation or contact on a daily basis without getting sick. Nonetheless, individuals with compromised immune systems are at a higher risk of developing an infection from these fungi.
Are Yeast Rashes Contagious? Unveiling The Truth
Yeast rashes, including Candida infections, are common among both adults and children. They can appear in various parts of the body, such as the mouth, skin folds, and genital areas. But are these yeast rashes contagious?
The good news is that yeast rashes are typically not contagious in the way that a cold or the flu is. You won’t catch a yeast rash from being around someone who has it, like you might catch a cold from a sneeze. However, there are some important factors to consider. While yeast rashes themselves may not be highly contagious, the fungi that cause them are naturally present on our skin. If someone has a weakened immune system, poor hygiene practices, or is in a warm and moist environment, these factors can contribute to the growth of yeast and potentially lead to an infection.
To prevent the spread of yeast infections and maintain healthy skin, it’s essential to practice good hygiene. This includes maintaining the affected areas clean and dry, using appropriate antifungal creams if recommended by a doctor, and avoiding tight-fitting clothing that can trap moisture.
Remember: Not all rashes are fungal, and not all rashes are contagious. So, it’s always best to get any rash checked by a doctor to know for sure.
Home Remedies For Fungal Rashes
1. Tea Tree Oil
Tea tree oil has antifungal properties and can be diluted with a carrier oil (like coconut oil) before applying it to the affected area. It’s important to do a patch test first, as some people might be sensitive to tea tree oil.
2. Turmeric Paste
Turmeric has anti-inflammatory and antimicrobial properties. Create a paste using turmeric powder and water, and apply it to the affected area for a short period of time (it can stain the skin).
3. Garlic
Garlic has natural antifungal properties. People who consume garlic regularly are less susceptible to fungal infections.
Crush a few cloves of garlic and mix with a carrier oil, then apply it to the rash. Be cautious, as garlic can be irritating to the skin for some people.
4. Coconut Oil and Aloe Vera
Both coconut oil and aloe vera have soothing properties and may provide relief from itching and inflammation associated with fungal rashes.
Aloe vera offers effective healing for fungal infections. Its antiseptic properties combat fungi and bacteria and can even restrict yeast growth, making it a fantastic at-home solution for fungal infections.
5. Oregano Oil
Oregano oil contains compounds like carvacrol that have antifungal properties. Mix a few drops with a carrier oil and apply it sparingly to the rash.
6. Apple Cider Vinegar
Apple cider vinegar may help restore the skin’s pH balance and create an unfavorable environment for fungi.
You can try consuming diluted apple cider vinegar, which might fight infections and support your body internally. Mix 1-2 tablespoons of apple cider vinegar with one cup of water.
Applying diluted apple cider vinegar directly to affected spots may speed up healing. For foot infections, soak your feet in a diluted solution of apple cider vinegar and water.
7. Baking Soda
Baking soda has antifungal properties and can help absorb moisture from the affected area. Create a paste with baking soda and water, and apply it to the rash.
8. Calendula
Calendula has soothing and anti-inflammatory properties. Calendula creams or ointments can be applied to the rash to help with irritation.
9. Grapefruit Seed Extract
Grapefruit seed extract is believed to have antifungal properties. Dilute a few drops with water and apply it to the affected area.
10. Licorice Root
Licorice naturally contains anti-inflammatory and anti-microbial properties, which make it great for fighting fungal infections.
To use it, put powdered licorice in a cup of water and heat it until it boils. Let it simmer for a while. Once it becomes like a paste, let it cool down and put this mixture on the affected skin two times a day.
11. Neem Oil
Neem oil is derived from the neem tree and has antimicrobial properties. Dilute neem oil with a carrier oil and apply it to the affected area.
You can also boil a few neem leaves in water and wash the infected areas.
12. Lavender Oil
Lavender oil has mild antifungal properties and can be diluted with a carrier oil before applying it to the rash. It’s also known for its soothing aroma.
13. Chamomile
Chamomile has anti-inflammatory and soothing properties. You can brew chamomile tea, let it cool, and then use it as a compress on the rash.
14. Honey
Raw honey has natural antifungal properties and can also help soothe the skin. Apply a thin layer of honey to the rash, let it sit for a short time, and then rinse it off.
15. Essential Oil Blends
Some essential oils, like a combination of thyme, cinnamon, and clove oils, are thought to have potent antifungal properties. However, essential oils are concentrated and should be used with caution and proper dilution.
16. Witch Hazel
Witch hazel has astringent properties and can help with itching and inflammation. Apply witch hazel extract to a cotton ball and gently dab it on the rash.
17. Epsom Salt Bath
Soaking in a warm bath with Epsom salts can help soothe irritated skin. Epsom salts also have potential antifungal properties.
18. Vinegar Soak
Apart from apple cider vinegar, white vinegar can also be diluted in water and used as a foot soak or applied with a cotton ball to the affected area.
19. Yogurt and Probiotics
Yogurt and other probiotics have lots of helpful bacteria that can keep away fungal infections. These good bacteria fight against the tiny germs that cause these infections.
Foods that are fermented also have these helpful bacteria. If these foods don’t work, you can try taking probiotic pills. These pills have more of the good bacteria packed into them.
Some people claim that the live cultures in yogurt can help restore the natural balance of skin flora. Apply plain, unsweetened yogurt to the rash and let it sit for a short time before rinsing.
20. Lemongrass
Lemongrass is also full of anti-microbial properties, so you can use it as one of the home remedies for your fungal infection. Mix lemongrass oil with another oil and put it on the infected area using a cotton ball or swab two or three times a day.
Remember: These remedies might not work for everyone, and there’s a risk of adverse reactions or interactions with existing conditions or medications. It’s important to be cautious and consult a healthcare professional if your fungal rash persists or worsens. Additionally, good hygiene practices, such as keeping the area clean and dry, wearing breathable fabrics, and avoiding tight clothing, can also help prevent and manage fungal rashes.
Preventing Fungal Rashes: Tips For Clear and Healthy Skin
Prevention is the key when it comes to fungal rashes. By adopting certain habits, you can reduce the risk of developing these uncomfortable skin conditions.
- Fungi thrive in moist environments, so keeping your skin dry is essential. After bathing or swimming, make sure to thoroughly dry your skin, especially in areas prone to rashes.
- Regularly wash your body with mild soap and water. Pay special attention to areas that tend to get sweaty or are prone to rashes, such as the armpits, groin, and feet.
- Wear clothing made from natural, breathable fabrics like cotton. This allows your skin to breathe and reduces the risk of moisture buildup.
- Refrain from using strong detergents when washing clothes.
- Resist the urge to scratch the affected area, as this can exacerbate the infection and heighten the risk of spread.
- Ensure the infected area is cleansed 2 to 3 times daily; adhering to this practice can help control and mitigate the extent of fungal growth.
- Fungal infections can spread through shared items like towels, socks, and shoes. Avoid sharing these items to minimize the risk of contagion.
- If you suspect a fungal rash, consult a healthcare professional. They may recommend antifungal creams or ointments to treat the infection. Follow their instructions for the best results.
Maintaining Skin Health: Hygiene And Beyond
Healthy skin goes beyond just preventing fungal rashes; it’s about overall skin hygiene and care. Even if you’ve never experienced a fungal rash, following these practices can help maintain radiant and healthy skin:
- Stay hydrated. Drink plenty of water. Your skin, just like any other part of your body, needs hydration to stay healthy.
- Eat a balanced diet. Nutrient-rich foods like fruits, vegetables, and whole grains support skin health from the inside out.
- Protect your skin. Use sunscreen to protect your skin from harmful UV rays and prevent sun damage. Always use sunscreen, even on cloudy days.
- Avoid harsh products. Choose gentle skincare products that won’t strip your skin of its natural oils.
How To Deal With A Fungal Rash
If you think you have a fungal rash:
- Consult a Doctor: Before you start any treatment, it’s important to make sure it’s really a fungal rash. Your doctor can guide you best.
- Topical Antifungals: These are creams or lotions that you can apply directly to the rash. They help kill the fungi causing the trouble.
- Keep it Dry: Fungi love moist environments. Dry your skin thoroughly after bathing, especially in areas that are prone to fungal infections.
- Avoid Sharing Personal Items: Until your rash is fully healed, make sure not to share towels, shoes, or clothes.
When To Seek Help: Consulting A Professional
- If you notice any unusual changes in your skin.
- If you’ve tried home remedies but don’t see any improvement.
- The fungal infection gets worse or keeps coming back.
- The infection starts to spread to other areas.
- If you experience persistent itching, redness, or discomfort.
- If you get a fungal infection while you’re pregnant.
- If you have diabetes and get a fungal infection.
- If the fungal infection comes with a fever or pus coming out.
Conclusion: Empowering Healthy Skin Knowledge
Understanding whether fungal rashes are contagious is crucial for maintaining clear and healthy skin. Yeast rashes like Candida infections are typically not highly contagious, but good hygiene practices are still important. Fungal skin infections caused by dermatophytes can spread and require careful prevention methods.
By following proper hygiene, using antifungal treatments when needed, and practicing healthy habits, you can take charge of your skin’s well-being. Remember, a combination of prevention, awareness, and self-care is the key to enjoying skin that’s not only clear but also vibrant and radiant.
Read more about Managing Contagious Viral Rashes
FAQs
Q: Are fungal rashes contagious?
A: Yes, fungal rashes can be contagious. Fungi causing these rashes can spread through direct contact with an infected person, contaminated objects, or surfaces. It’s important to take precautions and avoid sharing personal items to prevent spreading the infection to others.
Q: How do fungal rashes spread?
A: Fungal rashes spread through direct contact with an infected person, contaminated objects like towels or clothes, or surfaces where the fungi thrive. Touching or sharing items with an infected person can lead to the transmission of the fungal infection.
Q: Can I pass my fungal rash to someone else?
A: Unfortunately, yes. Fungal rashes are contagious, and they can spread through skin-to-skin contact, sharing personal items, or contact with surfaces that harbor the fungi. Proper hygiene and avoiding close contact can help prevent passing the infection to others.
Q: What precautions should I take if I have a fungal rash?
A: To prevent spreading the fungal rash, avoid close contact with others, don’t share personal items like towels or clothing, keep the affected area covered, and practice good hand hygiene. Prompt treatment and following medical advice can help minimize the risk of transmission.
Q: Can I go to work or school with a fungal rash?
A: It’s best to avoid close contact with others until your fungal rash is treated and under control. Many fungal rashes are contagious, so staying home until you’ve received appropriate treatment and your doctor gives the green light can help prevent the spreading of the infection.
Q: Can pets spread fungal rashes to humans?
A: Yes, some types of fungi causing rashes can be transmitted from pets to humans. Close contact with an infected pet’s skin, fur, or environment can lead to fungal transmission. It’s important to maintain good pet hygiene and consult a veterinarian if you suspect your pet has a fungal infection.
Q: How can I prevent spreading a fungal rash to my family?
A: Prevent spreading the fungal rash by not sharing personal items, washing your hands frequently, covering the affected area, and avoiding close contact. Launder your clothes and towels separately and maintain proper hygiene to reduce the risk of transmission to family members.
Q: Can over-the-counter antifungal creams help prevent contagion?
A: Over-the-counter antifungal creams can help treat fungal rashes, but their primary purpose is to alleviate the infection in the affected person. Preventing contagion involves practicing good hygiene, avoiding contact with infected individuals or items, and seeking proper medical advice for both treatment and prevention.
Q: When is it safe to be around others if I have a fungal rash?
A: It’s safe to be around others once your fungal rash is treated, showing signs of improvement, and your healthcare provider confirms that it’s no longer contagious. Adhering to their advice and completing the recommended treatment duration will help ensure the infection is under control.
Q: Is it necessary to see a doctor for a contagious fungal rash?
A: Yes, it’s recommended to consult a doctor for a contagious fungal rash. Proper diagnosis and treatment are crucial to prevent the spread of the infection. A doctor can also provide guidance on how to manage the infection, minimize transmission, and ensure a timely recovery.
References
https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/tinea-infection.html
https://www.msdmanuals.com/en-au/home/infections/fungal-infections/overview-of-fungal-infections
https://www.webmd.com/skin-problems-and-treatments/fungal-infections-skin