10 Acute Bacterial Skin Infections You Should Never Take It Easy!

When we hear the phrase “acute bacterial skin infections,” we often take it lightly, writing it off as nothing more than a minor nuisance. But the reality is that these infections can be incredibly life-threatening and should never be taken lightly – even if the symptoms seem relatively benign.
In this blog, we’ll explore several acute bacterial skin infections you should be aware of and take seriously. By understanding the signs, symptoms, and potential risks associated with such infections, you can guard yourself and your loved ones against any health concerns that may occur. Let’s get started!
Table of Contents
- Understanding Acute Bacterial Skin Infections
- Common Types Of Acute Skin Infections
- How To Recognize The Bacterial Infection Before It Becomes Serious?
- Natural Remedies For Acute Bacterial Skin Infections
- Antibiotics For Acute Bacterial Skin Infections
- When To Seek Medical Attention?
- Preventing Acute Bacterial Skin Infections
- In A Nutshell
Understanding Acute Bacterial Skin Infections
Acute bacterial skin infections are a common medical ailment that can cause a lot of pain and discomfort. They can vary in severity from mild to severe, depending on the type of bacteria that caused the infection and if it is localized or systemic. These infections are brought on by bacteria that can be either present on the skin all the time or gained from contact with other people or objects.
The most common types of acute bacterial skin infections include impetigo, cellulitis, folliculitis, and boils. These infections can affect anyone, regardless of age or gender. They often lead to symptoms such as redness, swelling, warmth, pain, and sometimes even the presence of pus.
Bacterial skin infections typically occur when bacteria enter the skin through a cut, scrape, insect bite, or even an area of dry or cracked skin. Sometimes, the bacteria are naturally present on the skin but multiply excessively due to certain conditions, like a weakened immune system or poor hygiene practices. In other cases, the bacteria come from external sources, such as contaminated objects or close contact with infected individuals.
Recognizing the signs of an acute bacterial skin infection is essential for early intervention. Keep an eye out for redness that expands outward, increasing warmth in the affected area, pain or tenderness, swelling, and the presence of pus or a yellowish crust. If you notice these symptoms, it’s crucial to seek medical aid for proper diagnosis and treatment.
Common Types Of Acute Skin Infections
When it comes to skin infections, the old phrase “better safe than sorry” definitely applies. Acute bacterial skin infections can range from mild to severe and even life-threatening, and it is significant to be aware of these infections and seek treatment as soon as possible.
Here are the most common to rare types of acute bacterial skin infections:
1. Folliculitis – When Hair Follicles Get Infected
Folliculitis denotes an infection of the hair follicles, which can be instigated by bacteria, such as Staphylococcus aureus or Pseudomonas aeruginosa. Symptoms usually include red, swollen, and tender bumps on the skin. However, they may also appear to be white or yellow in color.

Treatment for folliculitis involves antibiotics and keeping the affected area clean and dry.
2. Cellulitis – A Deceptive Skin Infection
Cellulitis is a common bacterial infection that affects the deeper layers of the skin. It usually appears as redness, swelling, and warmth in the affected area. You may also experience pain and a spreading rash. Cellulitis often occurs when bacteria enter the skin through a cut, scrape, or insect bite.

Prompt medical attention is necessary to arrest the infection from spreading and inducing more serious complications.
3. Impetigo – Contagious and Annoying
Impetigo is highly contagious and commonly affects children. It’s characterized by red sores that burst and leave a yellowish crust. These sores can erupt anywhere on the body but are most often found around the nose and mouth.

Impetigo spreads easily through direct contact or by sharing personal items. Prompt treatment with antibiotics is crucial to control the infection and prevent its transmission to others.
4. Erythrasma – Superficial Bacterial Infection
Erythrasma is a superficial bacterial infection that affects the skin folds in the armpits, groin, or between the toes. It typically presents as reddish-brown patches with slightly raised edges.
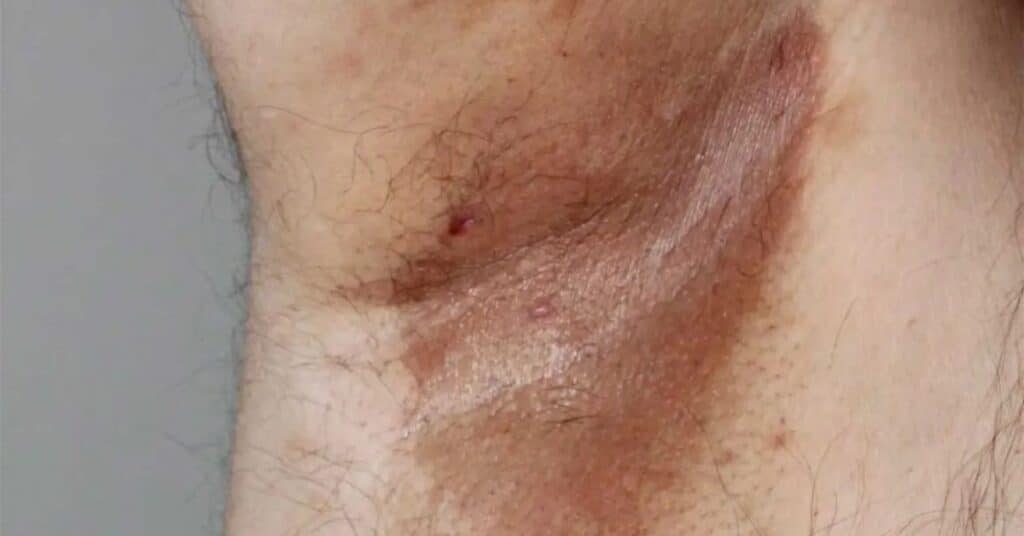
Good hygiene practices and keeping the affected areas clean and dry are key to managing and preventing erythrasma.
5. MRSA – Highly Contagious and Resistant to Certain Antibiotics
MRSA (Methicillin-Resistant Staphylococcus Aureus) is a common form of Staphylococcus infection that is resistant to certain antibiotics. This kind of bacterial infection is highly contagious and can be grievous if not treated quickly. Common symptoms, which can range from mild to severe, include red, swollen, and tender skin, fever, and fatigue.

Treatment involves the use of appropriate antibiotics.
6. Carbuncle – Collection of Pus Under the Skin
A carbuncle is a cluster of pus-filled boils that often occur along the back or shoulders. Caused by a bacterial infection, these boils are often very painful.

Treatment for carbuncles typically includes antibiotics, as well as the careful lancing and draining of the boils.
7. Staphylococcal Scalded Skin Syndrome (SSSS) – Severe and Life-Threatening Infection
SSSS is a rare but serious bacterial infection that primarily affects infants and young children. It starts with redness and tenderness of the skin, similar to a burn, and then progresses to widespread peeling. It’s caused by Staphylococcus aureus bacteria and often occurs in individuals with weakened immune systems.

Hospitalization and intravenous antibiotics are usually required for treatment.
8. Erysipelas – A Skin Infection with a Distinctive Appearance
Erysipelas is another bacterial infection that is characterized by a bright red and painful rash. It is most often caused by streptococcus bacteria and typically affects the face, but can also affect other areas of the body.

Treatment will involve antibiotics, which can be either oral or intravenous.
9. Boils – Painful and Pus-Filled Bumps
Boils are painful, pus-filled bumps that develop deep within the skin. They often start as a red, tender lump and gradually increase in size. Boils are usually caused by Staphylococcus aureus bacteria and can occur anywhere on the body. Avoid squeezing or popping boils, as this can lead to further infection.

Applying warm compresses can help alleviate the pain and promote drainage. In some cases, a healthcare professional may need to drain the boil.
10. Necrotizing Fasciitis – Rapidly Destroys the Body’s Soft Tissue
Necrotizing fasciitis, a.k.a. flesh-eating bacteria, is a rare but life-threatening infection that rapidly destroys the body’s soft tissue. It typically enters the body through a wound and spreads quickly.
Symptoms include severe pain, swelling, redness, and a rapidly spreading area of discolored skin. Immediate medical attention is pivotal in cases of necrotizing fasciitis, as surgical intervention and intravenous antibiotics are often necessary.
If you experience any of these infections, it is imperative to seek prompt medical assistance in order to prevent any long-term complications. Never adopt a lax approach when it comes to treating acute bacterial skin infections – prompt treatment is essential!
How To Recognize The Bacterial Infection Before It Becomes Serious?
Bacterial infections can vary from mild to severe, and it’s important to recognize them early before they progress into more serious conditions. Being able to discern the signs and symptoms of a bacterial infection can help you seek prompt medical attention and prevent complications.
- Monitor for Localized Symptoms: Pay attention to any changes in the affected area. Look for common signs of a bacterial infection, such as redness, swelling, warmth, tenderness, or the presence of pus.
- Persistent or Worsening Symptoms: If the symptoms of the bacterial skin infection persist or worsen despite home care measures or over-the-counter treatments, it is important to consult a healthcare professional. They can assess the infection, determine the appropriate course of action, and prescribe necessary medications to address the underlying infection.
- Check for Systemic Symptoms: If you experience systemic symptoms such as fever, chills, fatigue, or general malaise, it may indicate that the infection has spread beyond the skin. Systemic symptoms suggest a more severe infection that requires medical evaluation and appropriate treatment.
- Observe Changes in Wound Appearance: If you have a wound, monitor its healing progress. If the wound becomes more red and swollen or starts to discharge pus, it may indicate a bacterial infection.
- Look for Spreading Redness or Streaks: Some bacterial infections can cause redness that spreads beyond the initial site. If you observe red streaks emanating from a wound or redness spreading to nearby areas, it could suggest an infection that is spreading through the lymphatic system.
- Pay Attention to Increasing Pain: If you encounter increasing pain in a specific area, it might be an indication of a bacterial infection. Persistent or worsening pain should not be disregarded and ought to prompt further assessment.
- Pay Attention to Systemic Symptoms in Children: Children may display particular indications of a bacterial infection. Look for symptoms such as irritability, poor feeding, decreased activity, or changes in behavior. These signs may suggest a systemic infection in children.
- Take into Account the Risk Factors: If you possess certain risk factors, such as a weakened immune system, chronic medical conditions, recent surgery, or open wounds, you might be more susceptible to bacterial infections. Remain vigilant and seek medical attention if you notice any signs or symptoms.
- Rely on Your Instincts: If you have a strong feeling that something is amiss or if you are experiencing unusual symptoms that worry you, it is always preferable to err on the side of caution and consult a healthcare professional.
If you spot any of these symptoms, it’s important to take action to prevent the infection from progressing.
Natural Remedies For Acute Bacterial Skin Infections
While medical intervention is often necessary for bacterial skin infections, certain natural remedies can complement conventional treatments. Here are a few options:
Warm Compress: The application of warm compresses to the affected region can help soothe pain, reduce swelling, and promote healing. Wet a clean cloth in warm water, squeeze out the excess, and gently apply it to the infected area for 10-15 minutes several times a day.
Tea Tree Oil: This oil possesses antimicrobial properties that can aid in combating bacterial infections. Dilute a small quantity (a few drops) of tea tree oil into a carrier oil, say cold-pressed virgin coconut oil or olive oil, and gently pat it on the affected area using a cotton swab. Repeat this a few times daily.
Garlic: Its natural antibacterial properties can help fight skin infections. Crush a few garlic cloves to release the active compounds, then apply the paste to the infected area. Let it stay for about 15-20 minutes before rinsing off with warm water. Repeat this process a few times daily.

Turmeric: Turmeric contains curcumin, a compound with antimicrobial and anti-inflammatory properties. Mix turmeric powder with water or honey and apply the paste on the affected area. Allow it to stay for about 20-30 minutes before rinsing off. Repeat this once or twice daily.
Honey: Due to its antibacterial properties, applying raw honey to the infected area may help inhibit bacterial growth and promote healing.
Aloe Vera: The application of aloe vera gel to the skin can have soothing effects and promote healing.
Remember, while natural remedies can provide relief and aid in the healing process, they should not replace medical treatment. Seek guidance from a healthcare practitioner prior to utilizing any natural remedies, especially if you have underlying health conditions or allergies.
Antibiotics For Acute Bacterial Skin Infections
In many cases, acute bacterial skin infections require antibiotics to eliminate the bacteria and promote healing. The selection of antibiotics is dependent on various factors, including infection type, severity, and the individual’s overall health.
Frequently Prescribed Antibiotics
Penicillin: Among the commonly used antibiotics are penicillin and its derivatives, like amoxicillin and ampicillin. They prove effective against certain bacterial skin infections caused by Streptococcus or Staphylococcus bacteria. These antibiotics disrupt the formation of bacterial cell walls, leading to the demise of the bacteria.
Cephalosporins: Another class of antibiotics, cephalosporins, such as cephalexin and cefazolin, exhibit effectiveness against a broad spectrum of bacteria commonly associated with skin infections. Their mechanism interferes with bacterial cell wall synthesis, ultimately resulting in bacterial demise.
Macrolides: For individuals allergic to penicillin or those facing infections resistant to other antibiotics, macrolide antibiotics, including erythromycin, clarithromycin, and azithromycin, are often prescribed. Macrolides inhibit bacterial protein synthesis, hindering bacterial growth and replication.
Fluoroquinolones: More severe or complicated skin infections often necessitate the use of fluoroquinolone antibiotics, like ciprofloxacin and levofloxacin. By disrupting bacterial DNA replication and synthesis, these antibiotics effectively eliminate the bacteria.
Tetracyclines: Bacterial skin infections, including acne, are frequently treated with tetracycline antibiotics such as doxycycline and minocycline. Apart from inhibiting bacterial protein synthesis, tetracyclines possess anti-inflammatory properties that aid in controlling the infection.
It’s important to take the prescribed antibiotics as directed and complete the full course of treatment, even if you start feeling better. This ensures that the infection is completely eradicated and reduces the risk of recurrence or antibiotic resistance.
Route of Administration
Antibiotics for acute bacterial skin infections can be administered through different routes, depending on the severity and extent of the infection. The most common routes include:
- Oral: Oral antibiotics are often prescribed for mild to moderate bacterial skin infections. They are convenient and effective in reaching systemic circulation to target the bacteria causing the infection.
- Topical: Topical antibiotics, such as creams, ointments, or gels, are applied directly to the affected skin. They are commonly used for superficial skin infections or to prevent infection in open wounds.
- Intravenous: In more severe cases or when oral antibiotics are not suitable, intravenous antibiotics may be administered in a hospital setting. Intravenous antibiotics allow for higher drug concentrations in the bloodstream and are effective in treating systemic or deep-seated infections.
Duration of Treatment
The duration of antibiotic treatment for acute bacterial skin infections varies depending on the type and severity of the infection, as well as individual factors. It is significant to complete the full course of antibiotics as prescribed by the healthcare professional, even if the symptoms improve or disappear before the treatment is finished.
Failure to complete the prescribed course can lead to incomplete eradication of the bacteria, recurrence of the infection, or antibiotic resistance.
Consultation with a Healthcare Professional
It is paramount to emphasize that the use of antibiotics for acute bacterial skin infections should be undertaken in consultation with a healthcare professional. They will assess the specific condition, perform appropriate diagnostic tests if needed, and determine the most suitable antibiotic and treatment regimen based on the individual’s circumstances.
When To Seek Medical Attention?
While some bacterial skin infections can be managed at home with proper care and treatment, there are instances when it’s crucial to seek medical attention. Here are some situations that warrant immediate medical attention:
- Worsening Symptoms: If your symptoms worsen or fail to improve after a few days of home care, it’s important to consult a healthcare professional.
- High Fever: If you develop a high fever and a skin infection, it may be a sign of a more profound condition necessitating medical intervention.
- Rapid Spreading: If the infection spreads rapidly or covers a large area of the body, immediate medical intervention is necessary.
- Compromised Immune System: In the event of a compromised immune system resulting from a medical condition, it’s essential to seek medical attention promptly.
- Severe Pain or Discomfort: If the pain associated with the infection becomes severe or affects your daily activities, it’s important to consult a healthcare professional.
Bear in mind; it’s always better to be safe than to regret. If you’re unsure about the severity or progression of a bacterial skin infection, don’t hesitate to seek the expertise of a healthcare professional for a thorough assessment and treatment.
Preventing Acute Bacterial Skin Infections
Prevention is indeed preferable to cure! You can adopt several straightforward measures to minimize the likelihood of acquiring acute bacterial skin infections.
Ensure regular cleansing of your skin by washing it with mild soap and warm water. Exercise caution with regard to cuts, scrapes, and insect bites, giving them proper cleaning and adequate coverage. Refrain from sharing personal items like the towels and razors, as these can serve as breeding grounds for bacteria.
Furthermore, upholding a healthy lifestyle, encompassing a well-balanced diet and consistent physical activity, will help fortify your immune system.
In A Nutshell
Understanding acute bacterial skin infections is the first step toward effective management and prevention. By recognizing the common types, knowing the early signs, considering natural remedies as complementary measures, understanding the role of antibiotics, and knowing when to seek medical attention, you can take charge of your skin health.
Remember, maintaining good hygiene practices, keeping your skin clean and dry, and seeking professional help when needed will substantially contribute to keeping bacterial skin infections at bay.
FAQs
Q: What are acute bacterial skin infections?
A: Acute bacterial skin infections occur when bacteria invade the skin and surrounding tissues. They can vary from mild to severe and are often characterized by symptoms such as redness, swelling, warmth, tenderness, and pus.
Q: What causes acute bacterial skin infections?
A: Acute bacterial skin infections are primarily caused by bacteria entering the skin through cuts, scrapes, insect bites, or other breaks in the skin’s barrier. Common bacteria responsible for these infections include Staphylococcus aureus and Streptococcus pyogenes.
Q: What are the symptoms of acute bacterial skin infections?
A: The symptoms of acute bacterial skin infections may vary contingent upon the specific type and severity of the infection. Common symptoms include redness, swelling, pain, warmth, tenderness, the formation of pus or fluid-filled blisters, and sometimes fever.
Q: How are acute bacterial skin infections diagnosed?
A: Diagnosis of acute bacterial skin infections is usually based on a physical examination of the affected area and a review of the symptoms. In some cases, a sample of the wound or the affected area may be collected for laboratory testing to identify the specific bacteria causing the infection.
Q: How are acute bacterial skin infections treated?
A: Treatment for acute bacterial skin infections typically requires the use of antibiotics to kill the bacteria causing the infection. The choice of antibiotics depends on the type and severity of the infection. In some cases, surgical drainage of abscesses or debridement of necrotic tissue may be necessary.
Q: Can you prevent acute bacterial skin infections?
A: Although it may not be feasible to completely prevent all bacterial skin infections, certain measures can help reduce the risk. These include practicing good hygiene, keeping the skin clean and dry, avoiding close contact with individuals who have active infections, and promptly treating any cuts or wounds.
Q: How long does it take to recover from an acute bacterial skin infection?
A: The recovery time for acute bacterial skin infections can vary depending on several factors, including the type and severity of the infection, the individual’s overall health, and the effectiveness of the treatment. Mild infections may resolve within a few days to a week, while more severe infections may require longer treatment and recovery periods.
Q: How do you get a bacterial skin infection?
A: Bacterial skin infections can be acquired through various means. Common routes of transmission include direct contact with infected individuals, contact with contaminated surfaces or objects, or the penetration of bacteria through cuts, abrasions, or insect bites on the skin.
Q: Is a bacterial skin infection contagious?
A: Yes, some bacterial skin infections can be contagious. The contagiousness depends on the specific bacteria causing the infection and the mode of transmission. It is vital to practice good hygiene, avoid sharing personal items, and take appropriate precautions to prevent the spread of infection to others.
Q: Can you die from a bacterial skin infection?
A: While most bacterial skin infections can be successfully treated with appropriate medical care, in rare cases, severe or untreated infections can lead to complications and, in extreme cases, be life-threatening. It is paramount to diligently seek immediate medical assistance for severe or worsening symptoms to prevent complications and ensure proper treatment.
References
https://www.health.ny.gov/diseases/communicable/athletic_skin_infections/bacterial.htm
https://www.uptodate.com/contents/skin-and-soft-tissue-infection-cellulitis-beyond-the-basics
https://www.cdc.gov/antibiotic-use/skin-infections.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2605859/
https://www.healthline.com/health/skin-infection#treatment





